Introduction
Obstructive sleep apnea (OSA) is a serious disorder of repetitive pharyngeal collapse during sleep due to decreased pharyngeal airway size because of craniofacial structure or body fat. Patients with OSA report snoring, witnessed apneas, waking up with a choking sensation, excessive daytime sleepiness, fatigue, tiredness, and headache.1 Moderate to severe OSA has been found to affect 50% males and 25% females in the middle-aged population.3
OSA is an emerging public health concern globally. It has been linked to several comorbidities like metabolic syndrome, diabetes mellitus, insulin resistance, hypertension, coronary artery disease, stroke, increased risk of vehicular accidents, and various psychiatric disorders.4
Causes of OSA
The predisposing factors of OSA can be divided into anatomical and physiological factors (Figure 1).1,3
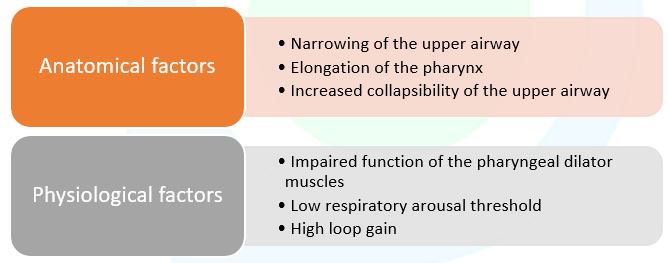
Figure 1: Etiological factors of OSA (Adapted from Whyte A et al. 2020)3
Risk factors for OSA
The Indian Initiative on Obstructive Sleep Apnea (INOSA) guidelines suggest the following risk factors linked to OSA (Figure 2).4
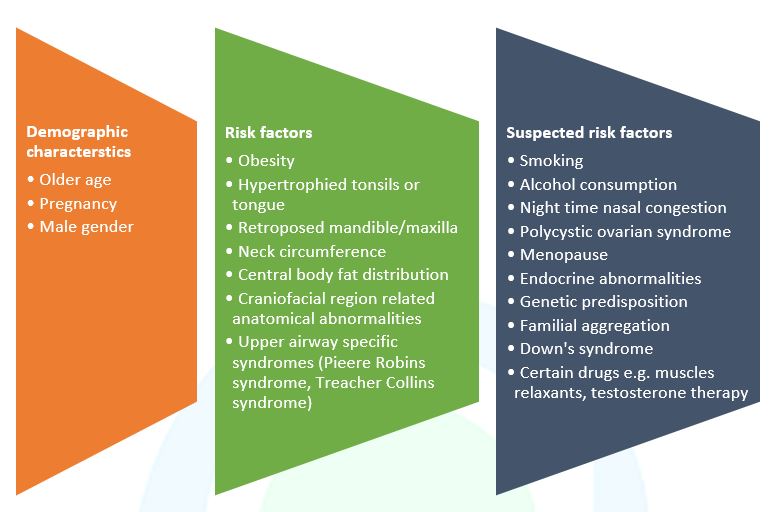
Figure 2. Factors that may contribute to OSA (Adapted from Sharma et al., 2014)4
Modification of certain risk factors can modulate the incidence of OSA
Hormonal changes: Males are more commonly affected than females, possibly due to hormonal effects on upper airway muscles and collapsibility. Post-menopausal women have a three times higher risk of developing OSA than premenopausal women due to dramatic changes in sex hormone levels.7
Obesity: Increased levels of cholesterols and obesity are major modifiable risk factors for sleep-related disorders, which predispose individuals to OSA due to mass loading in the upper airway.7
Smoking and alcohol: Smoking can cause airway inflammation and smoking-related diseases. Nicotine levels can also affect sleep stability. These effects of smoking could contribute to OSA. Alcohol consumption reduces motor output to the upper airways, causing hypotonia of the oropharyngeal muscles.7
Consequences of OSA on other systems
OSA significantly affects the social, emotional, and physical health of the patients. The consequences of OSA are characterized by overlapping symptoms such as lack of concentration, fatigue, loss of interest, and decreased libido.11 Figure 3 highlights the disease progression of OSA.3,5,6
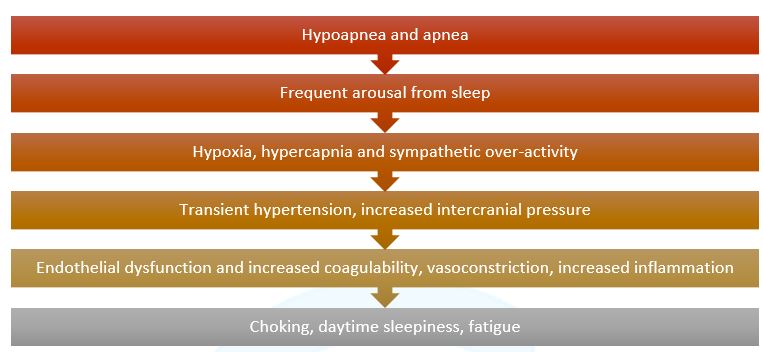
Figure 3. OSA disease progression (Source: Whyte A et al., 2020; Kim H et al., 2013; Arnaud C et al., 2020)3,5,6
The disease progression of OSA has a deleterious effect on various systems of the body (Figure 3).4
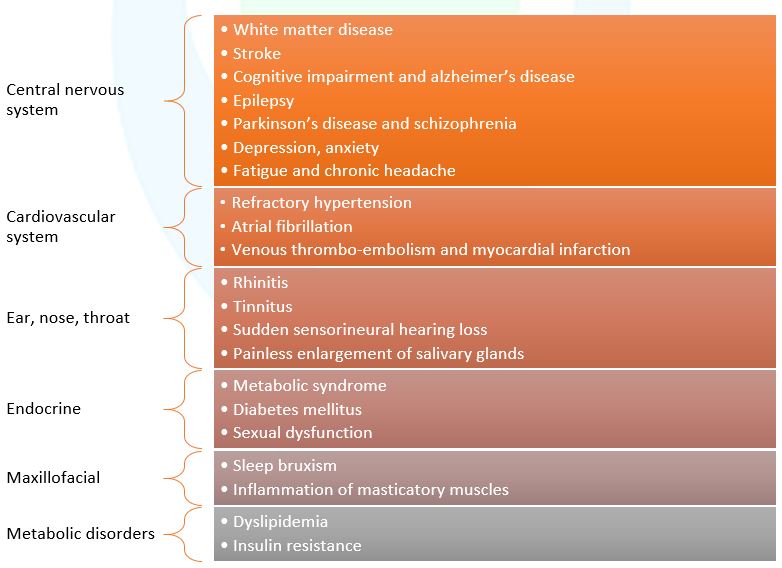
Figure 4. Complications of OSA (Adapted from Whyte A et al., 2020)3
OSA and comorbidities – A cross-linkage
A strong correlation exists between OSA and comorbidities due to common risk factors contributing to the etiology of one another.7
Hypertension: OSA is particularly common in patients with resistant hypertension. Evidence suggests that the chances of developing hypertension increase with a consecutive decline in nocturnal oxygen saturation.7
Cardiovascular diseases: The prevalence of OSA is high in patients with congestive heart failure. Recent studies suggest that the treatment of OSA in patients with congestive heart failure has improved symptoms over time.7
Stroke: OSA is highly prevalent in patients with stroke and transient ischemic attacks, leading to lower functional capacity and longer hospital stay.7
Diabetes Mellitus: Diabetes mellitus and OSA often coexist. Studies have demonstrated that poor metabolic and glycemic control have a significantly higher apnea-hypopnea index. Anti-diabetic medications, physical activity, and diet are reported to alleviate OSA-related effects.7,8
Conclusion
Obstructive sleep apnea significantly affects the quality of life and is associated with several long-term comorbidities. Therefore, spreading awareness about OSA and its proper diagnosis and treatment among the general population and healthcare practitioners is imperative